GDPR for Telehealth, the lawful basis, Data Subject Rights (DSR) workflows, Standard Contractual Clauses (SCCs), and patient consent are explained in clear language that both patients and providers can understand.
Table of Contents
- Introduction: Why GDPR Is Different in Healthcare
- What Telehealth Providers Must Know About GDPR
- Lawful Basis: Choosing the Right Legal Ground
- Data Subject Rights (DSR) Workflows Explained
- Standard Contractual Clauses (SCCs): Handling Data Across Borders
- Consent That Patients Actually Understand
- Security and Data Protection by Design
- Common Problems and Real-World Solutions
- GDPR vs HIPAA: Lessons for Clinics Serving Global Patients
- Practical Step-by-Step Playbook for Telehealth in EU/UK
- Country-Specific Notes: UK, Germany, France, Nordics
- Case Studies: Clinics That Did It Right
- Checklist for Ongoing Compliance
- Future of Telehealth Privacy in Europe
- Conclusion: Building Trust Through GDPR
1. Introduction: Why GDPR Is Different in Healthcare
Telehealth providers in Europe and the UK face GDPR compliance as their first and biggest hurdle. Unlike marketing or e-commerce, healthcare involves a special category data — patient health information.
That means:
- Higher responsibility for privacy.
- Clearer justification for data use.
- Stricter penalties for non-compliance.
Non-compliance can lead to fines of up to €20 million or 4% of global turnover, whichever is higher (ICO guidance).
In short: if you’re building or scaling a telehealth service, GDPR for Telehealth is not optional. It’s the backbone of patient trust.
2. What Telehealth Providers Must Know About GDPR
The General Data Protection Regulation (GDPR) applies to:
- Any clinic, startup, or hospital offering services to EU/UK patients.
- Any system processing EU/UK patient data, even if servers are abroad.
Key obligations for telehealth:
- Data minimization — collect only what you need.
- Purpose limitation — use data only for stated reasons.
- Accountability — document decisions and safeguards.
- Transparency — plain-language privacy notices.
Healthcare data is treated as special category data (Article 9 GDPR). That means extra safeguards and stronger justification for processing.
3. Lawful Basis: Choosing the Right Legal Ground
You can’t just process patient data “because it’s useful.” GDPR requires a lawful basis.
Most common for telehealth:
- Explicit Consent (Article 9(2)(a)) — patient agrees clearly.
- Provision of Healthcare (Article 9(2)(h)) — necessary for medical care.
- Public Interest in Healthcare (Article 9(2)(i)) — public health needs (e.g., pandemic).
Tip: Don’t rely on consent if you don’t need to. Patients can withdraw it. For ongoing care, use provision of healthcare as your legal ground.
Reference: EU GDPR Full Text
4. Data Subject Rights (DSR) Workflows Explained
Patients (data subjects) have rights under GDPR. Telehealth providers must operationalize these, not just mention them in a policy.
Rights to plan for:
- Right of access — patients request all data you hold.
- Right to rectification — correct errors in records.
- Right to erasure — delete data (unless medical retention applies).
- Right to data portability — transfer to another provider.
- Right to restrict or object — patients can limit certain uses.
Solution: Create DSR workflows:
- Online form for requests.
- Standard templates for responses.
- Deadline tracking (1 month max).
5. Standard Contractual Clauses (SCCs): Handling Data Across Borders
Telehealth often uses U.S. or non-EU vendors (EHR, cloud hosting, AI tools). That means data export.
GDPR requires:
- Adequacy decisions — if the country is approved by EU (e.g., UK, Switzerland).
- Standard Contractual Clauses (SCCs) — for other countries like the USA.
- Data Transfer Impact Assessments (DTIA) — assess vendor risks.
If you serve both EU and U.S. patients, you’ll likely combine HIPAA BAAs with GDPR SCCs.
Reference: European Commission SCC Guidance
6. Consent That Patients Actually Understand
Too many clinics use jargon-heavy privacy notices. Patients don’t understand them.
Best practices for telehealth consent:
- Use plain words: “We will use your data to provide medical care and keep your records.”
- Layered approach: short summary + full policy.
- Multiple languages (English, French, German, Arabic).
- Easy withdrawal: “Click here to withdraw consent.”
Tip: Record consent in your system (who, when, how).
7. Security and Data Protection by Design
GDPR requires data protection by design and by default.
For telehealth that means:
- Encryption: TLS 1.2+ for data in transit; AES-256 at rest.
- MFA & access controls for staff.
- Audit logs for patient access.
- Data minimization: no unnecessary fields.
- Privacy by default: sharing turned off unless needed.
Reference: NHS Digital Data Security Standards
8. Common Problems and Real-World Solutions
Problem 1: Using U.S. video platforms without SCCs.
- Solution: Sign SCCs or switch to EU-based vendor.
Problem 2: Doctors using WhatsApp for consultations.
- Solution: Move to HIPAA/GDPR-compliant telehealth platforms.
Problem 3: No process for data deletion.
- Solution: Create retention schedules; automate deletion after X years.
Problem 4: Over-reliance on consent.
- Solution: Use “provision of healthcare” as your main lawful basis.
9. GDPR vs HIPAA: Lessons for Clinics Serving Global Patients
- HIPAA (USA) = safeguards, BAAs, PHI.
- GDPR (EU/UK) = lawful basis, DSR rights, SCCs.
For global telehealth:
- Combine both.
- U.S. vendors: BAA + SCC.
- Patients: HIPAA Notice + GDPR privacy notice.
This makes your service globally trustworthy.
Reference: HHS HIPAA vs GDPR Overview
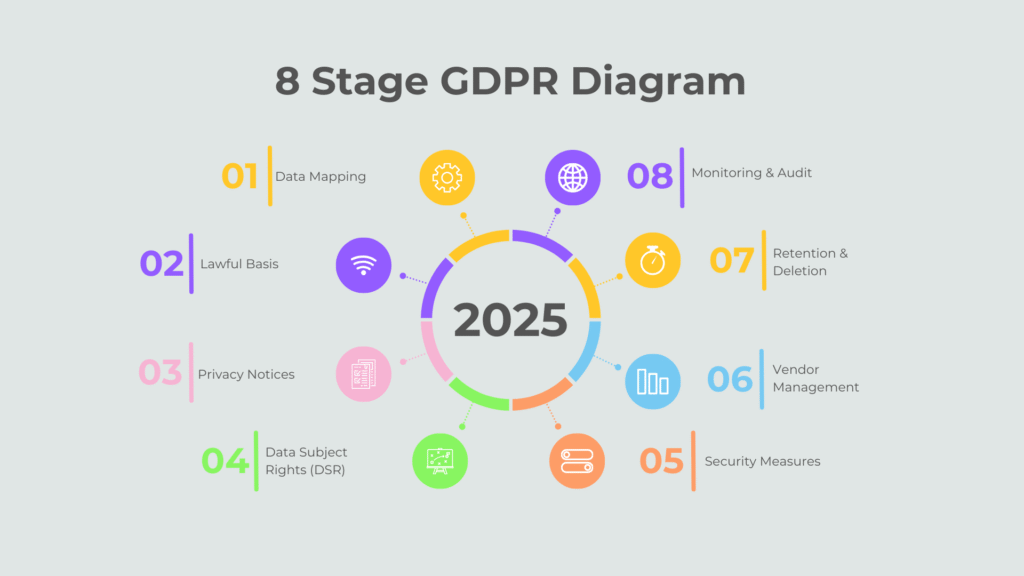
10. Practical Step-by-Step Playbook for Telehealth in EU/UK
- Map data flows (where data comes from, where it goes).
- Choose lawful basis (healthcare provision > consent).
- Update privacy notices (plain, multi-language).
- Set up DSR workflows (forms, templates, deadlines).
- Review vendors (BAAs + SCCs).
- Secure infrastructure (encryption, MFA, audit logs).
- Train staff (GDPR + cyber hygiene).
- Appoint DPO (if required by scale).
- Document everything (accountability principle).
- Test & audit (annual review).
11. Country-Specific Notes
- UK: GDPR + Data Protection Act 2018; ICO is regulator.
- Germany: strict; local authorities may enforce.
- France (CNIL): requires clear patient consent language.
- Nordics: emphasis on eHealth transparency portals.
12. Case Studies: Clinics That Did It Right
Case A — UK startup: Built GDPR workflows from day one; reduced patient complaints by 60%.
Case B — German telehealth provider: Switched video vendor to EU servers, passed regulator audit.
Case C — Multi-country platform: Combined HIPAA + GDPR policies, gained global trust.
13. Checklist for Ongoing Compliance
- Privacy notice updated
- Lawful basis documented
- SCCs signed
- DSR workflows tested
- Retention policy active
- Staff trained quarterly
- Annual audit done
14. Future of Telehealth Privacy in Europe
Expect:
- AI regulation (EU AI Act) — added safeguards for medical AI.
- Stricter fines for non-compliant startups.
- Patient empowerment — easier access to records.
- Cross-border care — need for harmonized rules.
15. Conclusion: Building Trust Through GDPR
Patients choose providers they trust. Trust is built when clinics show they respect privacy, follow GDPR, and explain it in simple words.
By applying this playbook, your clinic can:
- Avoid fines.
- Build credibility.
- Win more patients in EU/UK markets.
Focus Keyword Reminder:
This article showed why GDPR for Telehealth matters, how GDPR for Telehealth providers can comply, and gave a plain playbook to master GDPR for Telehealth in Europe & UK.
Explore More Expert Guides
We’ve created a complete library of resources to help clinics, hospitals, and healthcare providers grow online. From Local SEO for Clinics to Google Business Profile Optimization for Doctors, Digital Marketing Tips for Hospitals, and Patient Review Management Strategies, every article in our collection works together to give you a clear roadmap for building a powerful online presence. Visit our Healthcare Marketing Insights Hub to see all related posts and discover step-by-step solutions tailored to your practice.
Read more
- Clinic & Telehealth Technology
- ICO GDPR Guide
- EU GDPR Full Text
- NHS Digital Data Security Standards
- WHO Digital Health
- European Commission SCC Guidance
Lawful basis, Data Subject Rights (DSR) workflows, Standard Contractual Clauses (SCCs), and patient consent explained in clear language that patients and providers both understand.

Irfan Mangol is a professional web designer and Local SEO strategist specializing in Clinic & Telehealth Website Design for dermatology and cosmetic clinics across the USA.Inspired by insights from Moz, BrightLocal, and Search Engine Journal, he helps medical professionals boost patient engagement and rank higher ethically through strategic web design and SEO solutions.Learn more at irfanmangol.com.
Q1. What is Infermedica API used for in healthcare?
Infermedica API is an AI-powered tool for symptom checking, triage, and patient routing. It helps clinics screen patients online before booking appointments.
Q2. How can Infermedica API turn a clinic website into a patient screening hub?
By embedding the API, your website becomes a 24/7 front desk where patients can check symptoms, receive triage advice, and book the right service instantly.
Q3. Is Infermedica API HIPAA compliant?
Yes. Infermedica API supports HIPAA, GDPR, and other data protection rules, ensuring patient data is encrypted and processed securely.
Q4. Does Infermedica replace doctors or medical staff?
No. It only provides preliminary screening and triage. Doctors remain responsible for diagnosis and treatment.
Q5. Can Infermedica API be integrated with EHR systems?
Yes. Infermedica offers API hooks that can connect with most EHR, CRM, and booking systems, allowing symptom data to flow into patient records.
Q6. What are the benefits of using Infermedica for clinics?
1-Reduces staff workload
2-Improves booking accuracy
3-Cuts down patient no-shows
4-Builds patient trust with instant guidance
Q7. How much does Infermedica API cost?
Pricing depends on usage and number of API calls. Clinics typically pay a monthly subscription. Contact Infermedica for custom pricing.
Q8. Can patients use Infermedica API in multiple languages?
Yes. Infermedica supports multilingual screening (including English, Arabic, Russian, and more), making it ideal for international clinics.
Q9. Is the symptom checker safe for urgent cases?
Yes. The system flags urgent symptoms and advises immediate care, but it is not a substitute for emergency services.
Q10. What analytics does Infermedica provide to clinics?
It tracks symptom trends, patient journeys, and booking conversions, helping clinics improve operations and staffing.